Overstimulation and Sensory Overload in Adults and Children
Symptoms, causes, and evidence-based ways to regulate the nervous system
If you feel constantly on edge, mentally drained, easily irritated by noise or light, or physically unwell after busy days, you are not imagining it. Overstimulation is a genuine nervous system state, and it affects adults, teenagers, and children across Ireland far more often than most people realise.
This reference article is written by Claire Russell, a Counsellor and Psychotherapist, Clinical Medical Hypnotherapist, Clinical Hypnotherapist, RTT Therapist, Advanced RTT Practitioner, and Qualified Registered Nutritionist, with over 20 years of clinical experience working with adults, teens, and children ONLINE and in-person across Adare, Newcastle West, Limerick, Abbeyfeale, Charleville, Kanturk, Midleton, Youghal, Cork, Dublin, and Dungarvan.
Summary
Overstimulation, also known as sensory overload, occurs when the nervous system receives more sensory information than it can comfortably process. It commonly overlaps with anxiety, ADHD, autism, trauma responses, burnout, gut symptoms, hormonal changes, and chronic stress. Left unaddressed, it can affect mood, focus, sleep, digestion, relationships, and overall wellbeing. With the right therapeutic and nutritional support, the nervous system can learn to regulate more effectively.
What Is Overstimulation?
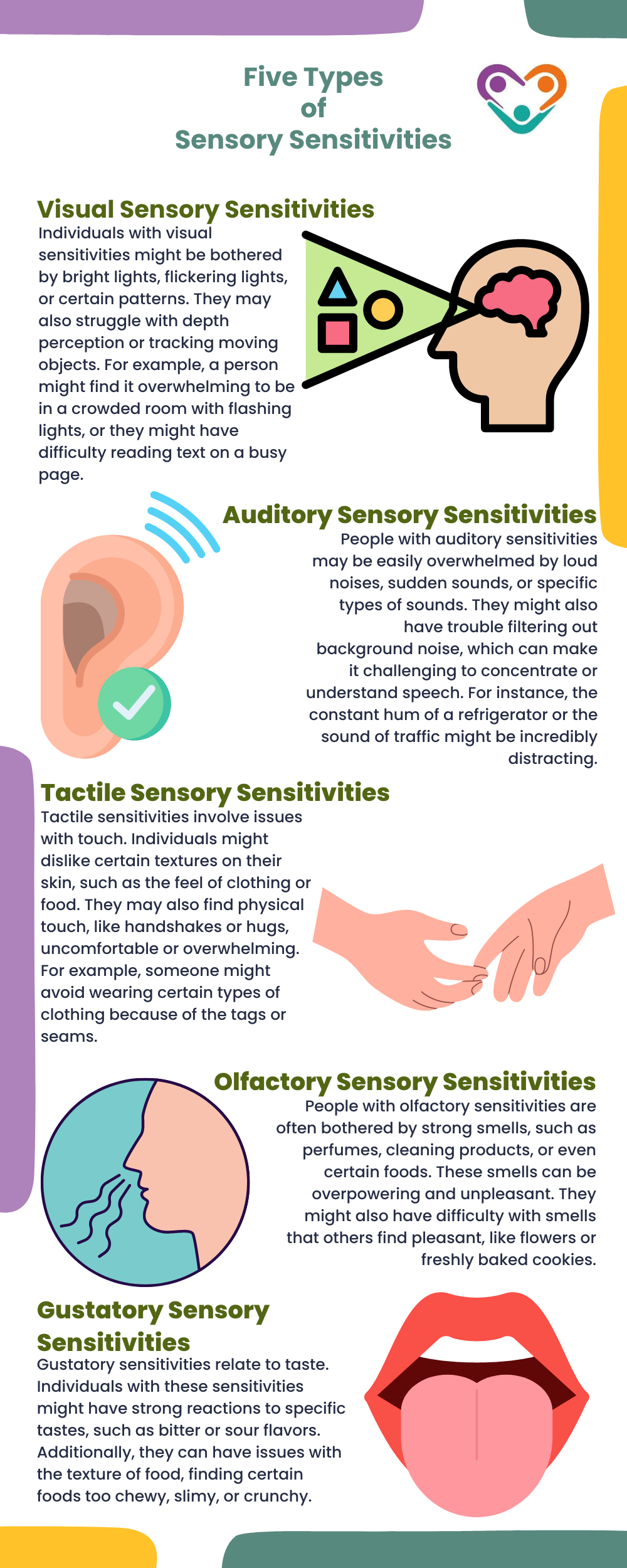
Overstimulation happens when your senses receive more input than your nervous system can manage at that moment. This input may include sound, light, touch, movement, visual clutter, social interaction, or digital information.
Your nervous system is designed to filter and prioritise information. When it becomes overloaded, it shifts into a state of protection. You may feel the urge to escape, shut down, react emotionally, or physically withdraw.
Tolerance for stimulation varies significantly. Factors such as sleep quality, stress levels, nutritional status, hormones, gut health, and past experiences all influence how much stimulation your system can handle on any given day.
Overstimulation vs Emotional Overwhelm
These terms are often used interchangeably, but clinically they describe different processes.
Overstimulation is primarily sensory and physiological. It arises from excessive input to the nervous system.
Overwhelm is more cognitive and emotional. It reflects mental overload from responsibility, pressure, or worry.
In practice, they frequently occur together. Overstimulation can intensify anxiety and emotional distress, while emotional stress can increase sensory sensitivity. This bidirectional loop is commonly seen in anxiety disorders, ADHD, trauma-related presentations, and burnout.
Everyday Situations That Trigger Overstimulation
Overstimulation does not require extreme environments. Many people experience it in ordinary settings, particularly when already stressed or depleted.
Common triggers include:
- Traffic noise and busy streets
- Open-plan workplaces with interruptions
- Classrooms with multiple voices and movement
- Shopping centres with bright lighting and visual clutter
- Public transport during peak hours
- Restaurants with echoing sound and overlapping conversations
- Screens with rapid movement, alerts, and notifications
- Multitasking and constant task switching
In clinical practice, many adults, teens and children report that even quiet environments can feel unbearable when their nervous system is already overloaded.
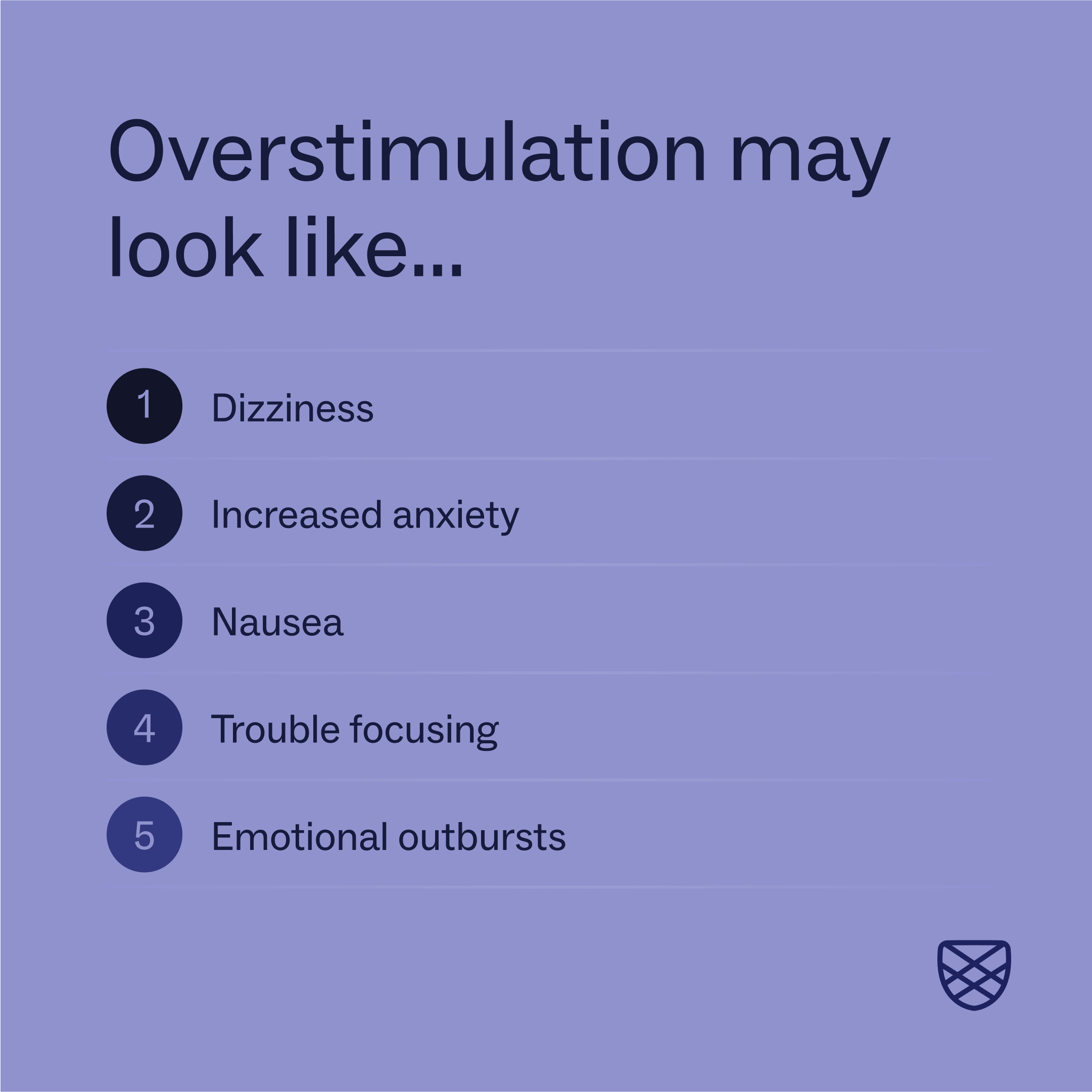
Symptoms of Overstimulation
Overstimulation affects the whole system. Symptoms vary between individuals and across life stages.
Physical symptoms
- Headaches or migraines
- Nausea or light-headedness
- Sweating or flushing
- Increased heart rate
- Muscle tension or trembling
- Digestive discomfort, bloating, or abdominal pain
Emotional symptoms
- Irritability or sudden anger
- Anxiety or inner restlessness
- Tearfulness or emotional volatility
- Withdrawal or shutdown
- Feeling unable to cope with small demands
Cognitive symptoms
- Difficulty concentrating
- Mental fog or confusion
- Memory difficulties
- Slower decision-making
- Mental exhaustion
Many people describe an urgent need to leave the environment to feel relief.
Overstimulation in Adults, Teens, and Children
Adults often internalise overstimulation. This may present as irritability, pacing, emotional withdrawal, increased reliance on caffeine or sugar, or difficulty sleeping.
Children and teenagers tend to express overstimulation more visibly. This may include meltdowns, hyperactivity, refusal, tearfulness, or behavioural changes. Teens may oscillate between agitation and complete shutdown.
Across more than 20 years of clinical experience, a consistent theme is that overstimulation is often misunderstood as defiance, laziness, or poor coping, rather than recognised as a nervous system response.
Who Is More Prone to Overstimulation?
Certain groups of adults, teens and children experience overstimulation more frequently than others including those with:
Anxiety disorders
Heightened alertness increases sensory reactivity.
ADHD
Difficulties filtering irrelevant stimuli can lead to rapid overload.
Autism spectrum presentations
Atypical sensory processing is common and may involve hypersensitivity or hyposensitivity frequently
Trauma and PTSD, and complex PTSD
Past threat and fears sensitises the nervous system, increasing reactivity to sensory cues.
Sensory processing difficulties
Challenges detecting, interpreting, or regulating sensory input.
Highly sensitive nervous systems
Some individuals naturally process information more deeply.
Hormonal shifts, chronic inflammation, autoimmune conditions, gut disturbances, and sleep disruption can significantly lower tolerance.
What Causes Overstimulation?
Overstimulation is rarely caused by one factor alone.
Common contributors include:
- Genetic sensory sensitivity
- Early life stress or trauma
- Chronic stress or burnout
- Excessive media and screen exposure
- Poor sleep or irregular routines
- Nutritional deficiencies and blood sugar instability
- High-noise or high-demand environments
- Caffeine, alcohol, or substance use
From a Registered Nutritionist perspective, unstable blood sugar, micronutrient deficiencies, and gut–brain axis disruption can significantly amplify nervous system reactivity.
The Impact of Chronic Overstimulation
When overstimulation becomes persistent, it can affect multiple areas of life.
Mental and emotional effects may include:
- Ongoing anxiety or irritability
- Emotional exhaustion and burnout
- Reduced frustration tolerance
- Relationship strain
- Reduced work or academic performance
Physical effects may include:
- Sleep disturbance or insomnia
- Elevated stress hormones
- Headaches and muscle pain
- Digestive symptoms
- Increased vulnerability to chronic health issues
How Overstimulation Is Addressed Therapeutically
Effective support focuses on regulation rather than avoidance alone.
In professional practice, support may include:
- Counselling and Psychotherapy to understand triggers, patterns, and emotional responses
- Clinical Medical Hypnotherapy and Clinical Hypnotherapy to support nervous system regulation
- RTT to address deeply embedded stress responses shaped by past experiences
- Hypnotherapy and other Hypnosis modalities for anxiety, sleep disruption, and emotional reactivity
- Registered Nutritionist support to stabilise blood sugar, inflammation, and gut–brain signalling
Support is available ONLINE or in person across Limerick, Cork, Dublin, Clare, and Munster.
Practical Strategies That Help Reduce Overstimulation
Helpful approaches focus on reducing load and improving recovery.
- Create calmer environments with softer lighting and reduced noise
- Establish predictable routines
- Limit multitasking and digital interruptions
- Take regular sensory breaks
- Support sleep and consistent meals
- Use sensory supports where appropriate
Strategies work best when tailored to the individual rather than applied rigidly.
When to Seek Professional Support
If overstimulation is frequent, intense, or affecting sleep, relationships, work, or mental health, professional support can make a meaningful difference. Assessment helps clarify whether anxiety, ADHD, trauma responses, hormonal changes, or nutritional factors are contributing.
Frequently Asked Questions
Is overstimulation a diagnosis?
No. It is a nervous system state that may occur alone or alongside other conditions.
Can overstimulation develop later in life?
Yes. Stress, illness, hormonal shifts, trauma, or burnout can lower tolerance over time.
Is overstimulation linked to gut issues?
Yes. The gut–brain axis means digestive distress can heighten nervous system reactivity.
Does overstimulation cause anxiety?
They influence each other. Either can intensify the other.
Can online therapy help with overstimulation?
For many people, yes. Online work can feel safer and less stimulating.
Educational Disclaimer
This article is for informative and educational purposes only and does not replace personalised medical or psychological care. Always consult a qualified professional regarding diagnosis or treatment.
Book a Consultation Now
If overstimulation, sensory overload, anxiety, ADHD, trauma responses, burnout, or emotional exhaustion are affecting your life, support is available.
Claire Russell Therapy
Counsellor and Psychotherapist
Clinical Medical Hypnotherapist
Clinical Hypnotherapist
Rapid Transformational Therapist (RTT)
Advanced Rapid Transformational Therapist
Qualified Registered Nutritionist
20+ years of clinical experience
087 616 6638
✉️ clairerusselltherapy@gmail.com
clairerusselltherapy.com
Appointments available ONLINE and in person in Adare, Newcastle West, Limerick, Abbeyfeale, Charleville, Kanturk, Fermoy, Tallow, Midleton, Youghal, Cork, Dublin, and Dungarvan.
Contact us today to discuss your needs
Scientific & Academic References
- McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1959220/ - Arnsten, A. F. T. (2009). Stress signalling pathways that impair prefrontal cortex structure and function.
https://www.nature.com/articles/nrn2648 - American Psychiatric Association. (2022). DSM-5-TR Diagnostic and Statistical Manual of Mental Disorders.
https://psychiatry.org/psychiatrists/practice/dsm - Miller, L. J., Anzalone, M. E., Lane, S. J., Cermak, S. A., & Osten, E. T. (2007). Concept evolution in sensory integration.
https://pubmed.ncbi.nlm.nih.gov/17436843/ - Ben-Sasson, A., et al. (2009). Sensory over-responsivity in children with autism spectrum disorders.
https://pubmed.ncbi.nlm.nih.gov/19360677/ - Tomchek, S. D., & Dunn, W. (2007). Sensory processing in children with and without autism.
https://pubmed.ncbi.nlm.nih.gov/17436841/ - Green, S. A., & Ben-Sasson, A. (2010). Anxiety disorders and sensory over-responsivity.
https://pubmed.ncbi.nlm.nih.gov/20014362/ - Bijlenga, D., et al. (2017). Sensory processing sensitivity in ADHD.
https://pubmed.ncbi.nlm.nih.gov/28199748/ - van der Kolk, B. A. (2014). The body keeps the score.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4010864/ - Thayer, J. F., & Lane, R. D. (2000). A model of neurovisceral integration in emotion regulation.
https://pubmed.ncbi.nlm.nih.gov/10668056/ - Porges, S. W. (2009). The polyvagal theory.
https://pubmed.ncbi.nlm.nih.gov/19259924/ - Ursin, H., & Eriksen, H. R. (2004). The cognitive activation theory of stress.
https://pubmed.ncbi.nlm.nih.gov/15504544/ - Acevedo, B. P., et al. (2014). The highly sensitive brain.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4086365/ - Teicher, M. H., & Samson, J. A. (2016). Annual research review: Enduring neurobiological effects of childhood abuse.
https://pubmed.ncbi.nlm.nih.gov/26693951/ - Holman, E. A., Garfin, D. R., & Silver, R. C. (2014). Media exposure and stress.
https://pubmed.ncbi.nlm.nih.gov/25125361/ - Shochat, T., et al. (2009). Sleep and sensory processing in children.
https://pubmed.ncbi.nlm.nih.gov/19448163/ - Szalma, J. L., & Hancock, P. A. (2011). Noise effects on human performance.
https://pubmed.ncbi.nlm.nih.gov/21358804/ - McEwen, B. S., & Gianaros, P. J. (2010). Central role of the brain in stress and adaptation.
https://pubmed.ncbi.nlm.nih.gov/20178752/ - Steptoe, A., & Kivimäki, M. (2012). Stress and cardiovascular disease.
https://pubmed.ncbi.nlm.nih.gov/22470147/ - Mayer, E. A., et al. (2015). Gut–brain axis.
https://pubmed.ncbi.nlm.nih.gov/25673227/ - Cryan, J. F., & Dinan, T. G. (2012). Mind-altering microorganisms.
https://pubmed.ncbi.nlm.nih.gov/22483040/ - Sapolsky, R. M. (2004). Why zebras don’t get ulcers.
https://www.sciencedirect.com/book/9780805073690/why-zebras-dont-get-ulcers - National Institute for Health and Care Excellence (NICE). (2019). Autism spectrum disorder in adults.
https://www.nice.org.uk/guidance/cg142 - National Institute of Mental Health. (2023). ADHD overview.
https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd - World Health Organization. (2022). Stress-related disorders and mental health.
https://www.who.int/teams/mental-health-and-substance-use